Lyme Disease
Dr Liegner is a physician caring for persons with Lyme disease,
tick-borne illnesses and related disorders.
— Dr Kenneth Liegner
Lyme disease is the most common vector-borne disease in the United States. Lyme disease is caused by the bacterium Borrelia burgdorferi. It is transmitted to humans chiefly through the bite of infected ticks.
Typical symptoms of Lyme disease include fever, headache, fatigue, and often, include a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, the heart, and the nervous system.
Lyme disease is diagnosed based on symptoms, physical findings, and the possibility of exposure to infected ticks. Laboratory testing is helpful if used correctly and performed with validated methods.
Sometimes called the new great imitator, Lyme disease, can present a variety of symptoms that mimic a wide range of illnesses, including chronic fatigue syndrome, fibromyalgia, Alzheimer's disease, depression, insomnia, autoimmune disorders such as rheum arthritis, lupus and multiple sclerosis.
Lyme Disease Event on Capitol Hill
Making the The Quiet Epidemic documentary about Lyme disease and bringing it to Capitol Hill was a dream of ours since this journey began in 2015, and in November 2024, it became a reality.
Senator Richard Blumenthal shared opening remarks before The Quiet Epidemic film presentation at the U.S. Capitol Visitor Center, on November 20, 2024. He discussed the challenges we're facing and how we can move forward, together, to solve the epidemic of Lyme:
A panel discussion brought together top experts in the field—researcher Monica Embers, Ph.D., investigative journalist Mary Beth Pfeiffer, board-certified internist Kenneth Liegner, M.D., microbiologist Holly Ahern, and attorney Ira Maurer, Esq. They discussed the science, the challenges facing patients, researchers and clinicians, and their personal stories of pushing forward despite the roadblocks.
Photography by Jiatong Lu
In Dr. Kenneth Liegner's words, during the film's post-screening Q&A,
we need a tidal wave to reach those who have the power to change the course of history for Lyme disease. By rallying leading nonprofits, patients, caregivers, celebrity advocates and even those who are not yet impacted, but care, we can create that tidal wave together.
Chronic Lyme Disease: An Evidence-Based Definition by the ILADS Working Group
Abstract: Objective: Chronic Lyme disease has been a poorly defined term and often dismissed as a fictitious entity. In this paper, the International Lyme and Associated Diseases Society (ILADS) provides its evidence-based definition of chronic Lyme disease. Definition: ILADS defines chronic Lyme disease (CLD) as a multisystem illness with a wide range of symptoms and/or signs that are either continuously or intermittently present for a minimum of six months. The illness is the result of an active and ongoing infection by any of several pathogenic members of the Borrelia burgdorferi sensu lato complex (Bbsl). The infection has variable latency periods and signs and symptoms may wax, wane and migrate. CLD has two subcategories, CLD, untreated (CLD-U) and CLD, previously treated (CLD-PT). The latter requires that CLD manifestations persist or recur following treatment and are present continuously or in a relapsing/remitting pattern for a duration of six months or more. Methods: Systematic review of over 250 peer reviewed papers in the international literature to characterize the clinical spectrum of CLD-U and CLD-PT. Conclusion: This evidence-based definition of chronic Lyme disease clarifies the term’s meaning and the literature review validates that chronic and ongoing Bbsl infections can result in chronic disease. Use of this CLD definition will promote a better understanding of the infection and facilitate future research of this infection.
THE QUIET EPIDEMIC (The Movie)
AFTER YEARS OF LIVING WITH MYSTERIOUS SYMPTOMS,
a young girl from Brooklyn and a Duke University scientist are diagnosed with a disease said to not exist: Chronic Lyme disease. The Quiet Epidemic follows their search for answers, which lands them in the middle of a vicious medical debate. What begins as a patient story evolves into an investigation into the history of Lyme disease, dating back to its discovery in 1975. A paper trail of suppressed scientific research, and buried documents reveals why ticks — and the diseases they carry — have been allowed to quietly spread around the globe.
According to a new CDC estimate, 476,000 people are diagnosed with Lyme disease yearly in the United States alone. Even with prompt treatment, 10-20% of people go on to suffer long-term, debilitating symptoms. An unknown number of people remain undiagnosed and untreated for years, decades or even a lifetime. Without an accurate diagnostic test, the true scale of this epidemic remains unknown.
Documentary filmmaking has a proven track record of moving the needle on long-ignored social issues.
We made The Quiet Epidemic to communicate the challenges we face and the solutions we need—to audiences far beyond the Lyme community. Change can happen faster when more people care about our cause.
Watch the Movie Trailer Below.
Dr. Liegner is featured in the movie.
How I Became a Science Experiment
By Ross Douthat, NYTimes columnist (10.30.2021)
So that dissenting doctor — and others like him, and many researchers doing work on Lyme disease treatments outside the official line — saved my life. But I also saved my own life, because I was the only one who could actually tell what treatments made a difference. So I had to act like a doctor or researcher myself, reading online for ideas and theories about drugs and supplements, mixing and matching to gauge my body’s reaction to different combinations — like a scientist working on a study with a sample size, an “n,” of only one.
FROM: The Harvard Gazette
New York Times columnist Ross Douthat ’02 writes candidly about his five-year struggle with Lyme disease in his wrenching and vivid book. The Gazette spoke with Douthat about the lessons he learned about himself and other people’s suffering, the controversy around Lyme, and how he finally managed to control his illness and recover. This interview was edited for clarity and length.
GAZETTE:
What are the most common misconceptions about Lyme disease?
DOUTHAT:
There are two related misconceptions.
The first is that it’s a simple matter to treat; that all you have to do is take four to six weeks of antibiotics and you should automatically feel better. This is a common belief because it’s true; 80 to 85 percent of people who get Lyme disease can treat it and get better very quickly. But then there is a substantial population for whom that short treatment doesn’t work, and they end up with long-term symptoms that the existing scientific consensus doesn’t know how to treat. The basic problem is the gap between the simplicity of treatment for the majority and the incredible difficulty of treatment for a small but substantial minority.
The other misconception is not just about chronic Lyme disease, but about chronic illness in general. There is a sense, when you haven’t lived through this kind of experience yourself, that having a chronic illness is just a slightly worse version of people’s everyday struggles. People with chronic illness will report that they have headaches or sleeping problems or fatigue and people who aren’t sick hear them and think, “Well, that sounds like what everybody goes through sometimes.” And this then feeds into the sense that people with chronic problems are malingering, that they’re obsessed with their own symptoms, that they’re hypochondriacs, and all these kinds of cliches and stereotypes. Obviously, sometimes those stereotypes fit, but in most of the cases that make up what we call chronic Lyme disease, you’re dealing with something that is devastating, that is not just occasional fatigue or occasional headaches. It’s a pain that literally never leaves you alone. One reason I wrote the book was to try to convey some of that reality more clearly; that whatever is going on with chronic illness, whether it’s Lyme or long-haul COVID or chronic fatigue syndrome or anything else, it is a genuinely devastating problem for the people afflicted by it.
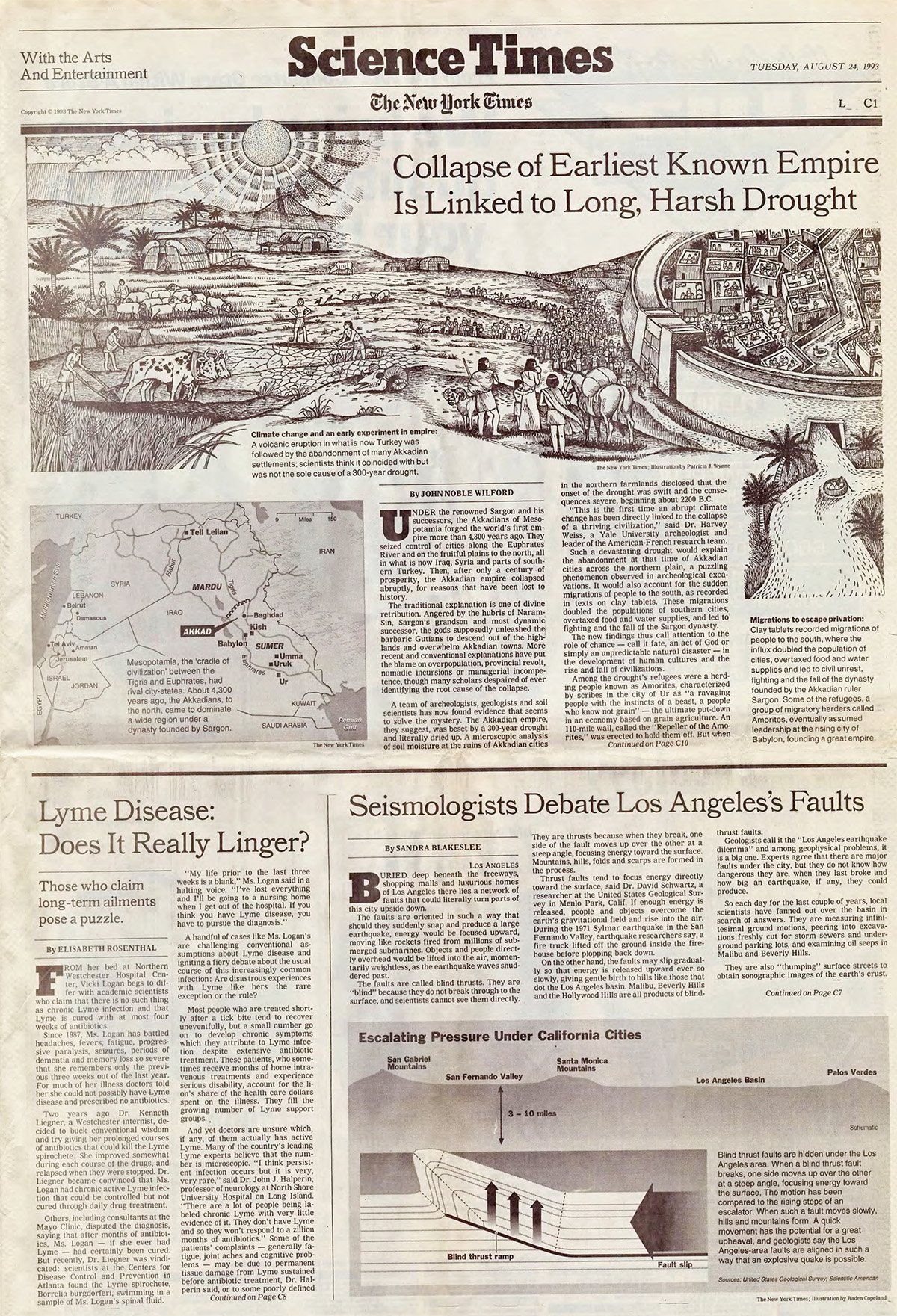
Lyme Disease: Does It Really Linger?
By Elisabeth Rosenthal. New York Times, Aug. 24, 1993
FROM her bed at Northern Westchester Hospital Center, Vicki Logan begs to differ with academic scientists who claim that there is no such thing as chronic Lyme infection and that Lyme is cured with at most four weeks of antibiotics.
Since 1987, Ms. Logan has battled headaches, fevers, fatigue, progressive paralysis, seizures, periods of dementia and memory loss so severe that she remembers only the previous three weeks out of the last year. For much of her illness doctors told her she could not possibly have Lyme disease and prescribed no antibiotics.
Two years ago Dr. Kenneth Liegner, a Westchester internist, decided to buck conventional wisdom and try giving her prolonged courses of antibiotics that could kill the Lyme spirochete: She improved somewhat during each course of the drugs, and relapsed when they were stopped. Dr. Liegner became convinced that Ms. Logan had chronic active Lyme infection that could be controlled but not cured through daily drug treatment.
Others, including consultants at the Mayo Clinic, disputed the diagnosis, saying that after months of antibiotics, Ms. Logan -- if she ever had Lyme --had certainly been cured. But recently, Dr. Liegner was vindicated: scientists at the Centers for Disease Control and Prevention in Atlanta found the Lyme spirochete, Borrelia burgdorferi, swimming in a sample of Ms. Logan's spinal fluid.
"My life prior to the last three weeks is a blank," Ms. Logan said in a halting voice. "I've lost everything and I'll be going to a nursing home when I get out of the hospital. If you think you have Lyme disease, you have to pursue the diagnosis."
A handful of cases like Ms. Logan's are challenging conventional assumptions about Lyme disease and igniting a fiery debate about the usual course of this increasingly common infection: Are disastrous experiences with Lyme like hers the rare exception or the rule?
Most people who are treated shortly after a tick bite tend to recover uneventfully, but a small number go on to develop chronic symptoms which they attribute to Lyme infection despite extensive antibiotic treatment. These patients, who sometimes receive months of home intravenous treatments and experience serious disability, account for the lion's share of the health care dollars spent on the illness. They fill the growing number of Lyme support groups.
And yet doctors are unsure which, if any, of them actually has active Lyme. Many of the country's leading Lyme experts believe that the number is microscopic. "I think persistent infection occurs but it is very, very rare," said Dr. John J. Halperin, professor of neurology at North Shore University Hospital on Long Island. "There are a lot of people being labeled chronic Lyme with very little evidence of it. They don't have Lyme and so they won't respond to a zillion months of antibiotics." Some of the patients' complaints --generally fatigue, joint aches and cognitive problems -- may be due to permanent tissue damage from Lyme sustained before antibiotic treatment, Dr. Halperin said, or to some poorly defined immune reaction set off by prior infection. He and many other doctors say they believe that the majority never had Lyme at all.
On the other side are Dr. Liegner and other doctors who say their practices are filled with Lyme patients who do not get better. They say academic experts are so blinded by what they "know" that they cannot see the evidence piling up in front of their eyes.
"I think that Lyme is an incurable disease in many patients -- there's no question in my mind about that -- and I think that's being suppressed and denied," Dr. Liegner said. "Cases like Vicki Logan's are not exceptions; they reveal the problems with our current paradigm.”
“Major initiative needed to fight tick-borne infections”
Dr Kenneth Liegner “Valley Views” in the Poughkeepsie Journal on August 22nd, 2012 is below.
Additional writings and articles
by Dr Liegner:
Lyme Disease: the Sensible Pursuit of Answers
By Kenneth B. Liegner
“In 1989, Preac-Mursic et al. published a landmark article documenting the recovery of living Bondella burdorferi by culture from patients who had been previously treated with regimens believed to cure the disease. Included was one patient who had been treated with 10 days of intravenous ceftriaxone and from whose spinal fluid the organism was grown following treatment”…
Click here to read the entire article
B. burgdorferi-Seek and Ye Shall Find Expanding the Envelope
By Kenneth B. Liegner
“The borreliae, present on this earth for eons, evolved alongside mammalian life forms in a host-parasiterelation- ship, no doubt long before the appearanceof humankind. It should not surprise us, then, that we have much to learn about the range of diseases that the borreliae may underlie and the true scope of infection of the human inhabitants of this planet. We are at the threshold of a new and exciting era in the understanding and conquest of Lyme borreliosis”…
Click here to read the entire article
Dr Liegner’s letter to the Institute of Medicine in 2010:
“… Honest review of the worldwide peer-reviewed scientific literature reveals an abundance of evidence for the existence of chronic Lyme disease in humans and animals. Much of this evidence was presented to the Lyme Disease Review Panel of the Infectious Diseases Society of America on July 30, 2009. Regrettably, the panel chose to sustain the 2006 IDSA Lyme Disease Guidelines. IDSA leaders were defiant from the outset asserting the Connecticut Attorney General could make them review the guidelines but that he couldn’t make them change them. In retrospect it was a serious strategic error to leave the review process within the hands and ultimately under the control of the IDSA itself.
The standard of care set by the IDSA 2006 Lyme disease guidelines is one of medical neglect of persons suffering from chronic Lyme disease”…
Click here to read the entire letter
Recurrent erythema migrans despite extended antibiotic treatment with minocycline in a patient with persisting Borrelia burgdorferi infection
By Kenneth B. Liegner
Controversy exists about wether ongoing signs and symptoms in patients previously treated for Lyme disease are caused by persisting infections, or a combination of the two. We report a case that we believe emphasizes the stubborn and persisting nature if Borrelia burgdorferi infection.
Click here to read the entire article
Lyme disease: Overview & Review of the Literature (History, prepared 03.1988)
By Kenneth B. Liegner
Allan C. Steere and associates from Yale University recognized Lyme disease as a distinct entity in 1975. Steere was investigating an epidemic of what was originally believed to be Juvenile Rheumatoid Arthritis (JRA). An unusual cluster of arthritis in children and adults occurred, centered about the towns of Old Lyme and East Haddam, Connecticut.